 |

|
Overview Information
| Section 1: Understanding Addiction and Abuse |
| Section 2: Co-Occurring Disorders |
| Section 3: Substances; Names; Effects |
Understanding Addiction and Abuse
Many people do not understand why individuals become addicted to drugs or how drugs change the brain  to foster compulsive drug abuse. They mistakenly view drug abuse and addiction as strictly a social problem and may characterize those who take drugs as morally weak. One very common belief is that drug abusers should be able to just stop taking drugs if they are only willing to change their behavior. What people often underestimate is the complexity of drug addiction—that it is a disease that impacts the brain and because of that, stopping drug abuse is not simply a matter of willpower. Through scientific advances we now know much more about how exactly drugs work in the brain, and we also know that drug addiction can be successfully treated to help people stop abusing drugs and resume their productive lives. to foster compulsive drug abuse. They mistakenly view drug abuse and addiction as strictly a social problem and may characterize those who take drugs as morally weak. One very common belief is that drug abusers should be able to just stop taking drugs if they are only willing to change their behavior. What people often underestimate is the complexity of drug addiction—that it is a disease that impacts the brain and because of that, stopping drug abuse is not simply a matter of willpower. Through scientific advances we now know much more about how exactly drugs work in the brain, and we also know that drug addiction can be successfully treated to help people stop abusing drugs and resume their productive lives.
Drug abuse and addiction are a major burden to society. Estimates of the total overall costs of substance abuse in the United States—including health- and crime-related costs as well as losses in productivity—exceed half a trillion dollars annually. This includes approximately $181 billion for illicit drugs, $168 billion for tobacco, and $185 billion for alcohol. Staggering as these numbers are, however, they do not fully describe the breadth of deleterious public health—and safety—implications, which include family disintegration, loss of employment, failure in school, domestic violence, child abuse, and other crimes.
What is drug addiction?
Addiction is a chronic, often relapsing brain disease that causes compulsive drug seeking and use despite harmful consequences to the individual who is addicted and to those around them. Drug addiction is a brain disease because the abuse of drugs leads to changes in the structure and function of the brain. Although it is true that for most people the initial decision to take drugs is voluntary, over time the changes in the brain caused by repeated drug abuse can affect a person’s self control and ability to make sound decisions, and at the same time send intense impulses to take drugs.
It is because of these changes in the brain that it is so challenging for a person who is addicted to stop abusing drugs. Fortunately, there are treatments that help people to counteract addiction’s powerful disruptive effects and regain control. Research shows that combining addiction treatment medications, if available, with behavioral therapy is the best way to ensure success for most patients. Treatment approaches that are tailored to each patient’s drug abuse patterns and any co-occurring medical, psychiatric, and social problems can lead to sustained recovery and a life without drug abuse.
Similar to other chronic, relapsing diseases, such as diabetes, asthma, or heart disease, drug addiction can be managed successfully. And, as with other chronic diseases, it is not uncommon for a person to relapse and begin abusing drugs again. Relapse, however, does not signal failure—rather, it indicates that treatment should be reinstated, adjusted, or that alternate treatment is needed to help the individual regain control and recover.
What happens to your brain when you take drugs?
Drugs are chemicals that tap into the brain’s communication system and disrupt the way nerve cells normally send, receive, and process information. There are at least two ways that drugs are able to do this: (1) by imitating the brain’s natural chemical messengers, and/or (2) by overstimulating the “reward circuit” of the brain.
Some drugs, such as marijuana and heroin, have a similar structure to chemical messengers, called neurotransmitters, which are naturally produced by the brain. Because of this similarity, these drugs are able to “fool” the brain’s receptors and activate nerve cells to send abnormal messages.
Other drugs, such as cocaine or methamphetamine, can cause the nerve cells to release abnormally large amounts of natural neurotransmitters, or prevent the normal recycling of these brain chemicals, which is needed to shut off the signal between neurons. This disruption produces a greatly amplified message that ultimately disrupts normal communication patterns.
Nearly all drugs, directly or indirectly, target the brain’s reward system by flooding the circuit with dopamine. Dopamine is a neurotransmitter present in regions of the brain that control movement, emotion, motivation, and feelings of pleasure. The overstimulation of this system, which normally responds to natural behaviors that are linked to survival (eating, spending time with loved ones, etc.), produces euphoric effects in response to the drugs. This reaction sets in motion a pattern that “teaches” people to repeat the behavior of abusing drugs.
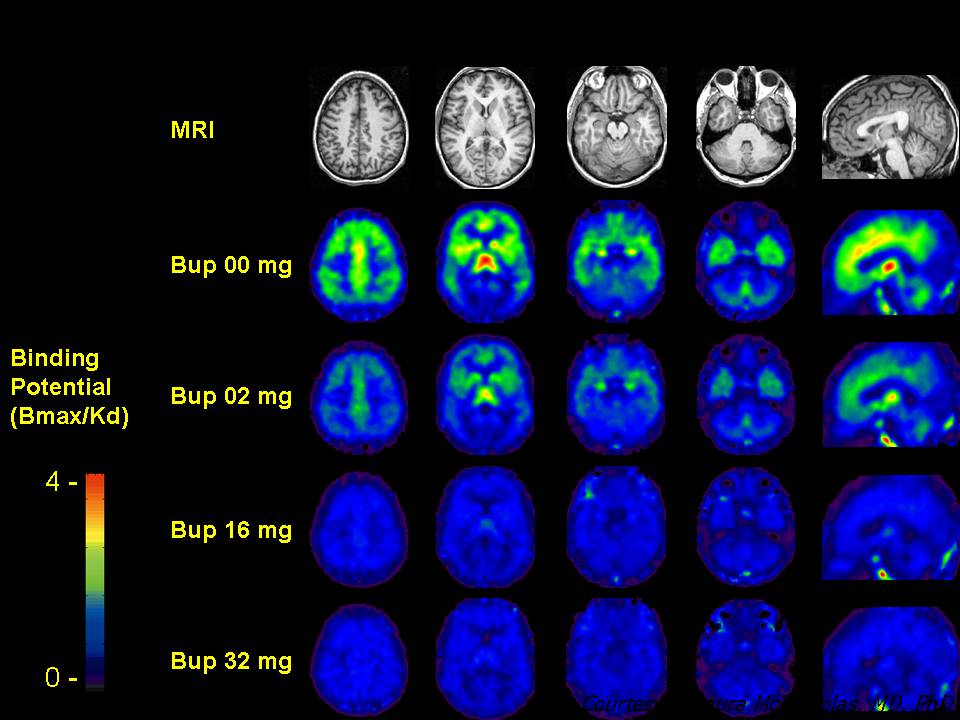
As a person continues to abuse drugs, the brain adapts to the overwhelming surges in dopamine by producing less dopamine or by reducing the number of dopamine receptors in the reward circuit. As a result, dopamine’s impact on the reward circuit is lessened, reducing the abuser’s ability to enjoy the drugs and the things that previously brought pleasure. This decrease compels those addicted to drugs to keep abusing drugs in order to attempt to bring their dopamine function back to normal. And, they may now require larger amounts of the drug than they first did to achieve the dopamine high—an effect known as tolerance.
Long-term abuse causes changes in other brain chemical systems and circuits as well. Glutamate is a neurotransmitter that influences the reward circuit and the ability to learn. When the optimal concentration of glutamate is altered by drug abuse, the brain attempts to compensate, which can impair cognitive function. Drugs of abuse facilitate nonconscious (conditioned) learning, which leads the user to experience uncontrollable cravings when they see a place or person they associate with the drug experience, even when the drug itself is not available. Brain imaging studies of drug-addicted individuals show changes in areas of the brain that are critical to judgment, decisionmaking, learning and memory, and behavior control. Together, these changes can drive an abuser to seek out and take drugs compulsively despite adverse consequences—in other words, to become addicted to drugs..jpg)
Why do some people become addicted, while others do not?
No single factor can predict whether or not a person will become addicted to drugs. Risk for addiction is influenced by a person’s biology, social environment, and age or stage of development. The more risk factors an individual has, the greater the chance that taking drugs can lead to addiction. For example:
- Biology. The genes that people are born with––in combination with environmental influences––account for about half of their addiction vulnerability. Additionally, gender, ethnicity, and the presence of other mental disorders may influence risk for drug abuse and addiction.
- Environment. A person’s environment includes many different influences––from family and friends to socioeconomic status and quality of life in general. Factors such as peer pressure, physical and sexual abuse, stress, and parental involvement can greatly influence the course of drug abuse and addiction in a person’s life.
- Development. Genetic and environmental factors interact with critical developmental stages in a person’s life to affect addiction vulnerability, and adolescents experience a double challenge. Although taking drugs at any age can lead to addiction, the earlier that drug use begins, the more likely it is to progress to more serious abuse. And because adolescents’ brains are still developing in the areas that govern decisionmaking, judgment, and self-control, they are especially prone to risk-taking behaviors, including trying drugs of abuse.
Co-occurring Disorders
What Is Comorbidity?
“Comorbidity” is a term used to describe two or more disorders or illnesses occurring in the same person. They can occur at the same time or one after the other. Comorbidity also implies interactions between the illnesses that can worsen the course of both.
Is Drug Addiction a Mental Illness?
Yes, addiction changes the brain in fundamental ways, disturbing a person’s normal hierarchy of needs and desires and substituting new priorities connected with procuring and using the drug. The resulting compulsive behaviors that weaken the ability to control impulses, despite the consequences, are similar to hallmarks of other mental illnesses.
How Common Are Comorbid Drug Addiction and Other Mental Illnesses?
Many people who are addicted to drugs are also diagnosed with other mental disorders and vice versa. For example, compared with the general population, people addicted to drugs are roughly twice as likely to suffer from mood and anxiety disorders, with the reverse also true.*
Why Do These Disorders Often Co-occur?
Although drug use disorders commonly occur with other mental illnesses, this does not mean that one caused the other, even if one appeared first. In fact, establishing causality or even directionality (i.e., which came first) can be difficult. However, research suggests the following possibilities for their co-occurrence:
Drug abuse may bring about symptoms of another mental illness. Increased risk of psychosis in some marijuana users suggests this possibility.
- Mental disorders can lead to drug abuse, possibly as a means of “self-medication.” Patients suffering from anxiety or depression may rely on alcohol, tobacco, and other drugs to temporarily alleviate their symptoms.
- These disorders could also be caused by common risk factors, such as—
-
- Overlapping genetic vulnerabilities. Common genetic factors may make a person susceptible to both addiction and other mental disorders or to having a greater risk of a second disorder once the first appears.
- Overlapping environmental triggers. Stress, trauma (such as physical or sexual abuse), and early exposure to drugs are common factors that can lead to addiction and other mental illnesses
- Involvement of similar brain regions. Brain systems that respond to reward and stress, for example, are affected by drugs of abuse and may show abnormalities in patients who have certain mental disorders.posure to drugs are common factors that can lead to addiction and other mental illnesses.
- Drug use disorders and other mental illnesses are developmental disorders. That means they often begin in the teen years or even younger—periods when the brain experiences dramatic developmental changes. Early exposure to drugs of abuse may change the brain in ways that increase the risk for mental disorders. Also, early symptoms of a mental disorder may indicate an increased risk for later drug use.
|
How Are These Comorbid Conditions Diagnosed and Treated?
The rate of comorbidity between drug use disorders and other mental illnesses calls for a comprehensive approach that identifies and evaluates both. Accordingly, anyone seeking help for either drug abuse/addiction or another mental disorder should be checked for both and treated accordingly.
There are several behavioral therapies that have shown promise for treating comorbid conditions. These approaches can be designed to target patients according to specific factors such as age or marital status: some therapies have proved more effective for adolescents, while others have shown greater effectiveness for adults; some therapies are designed for families and groups, others for individuals.
While several medications exist for treating addiction and other mental illnesses, most have not been studied in patients with comorbidities. For example, individuals addicted to heroin, prescription pain medications, cigarettes, or alcohol can be treated with appropriate medications to ease withdrawal symptoms and drug craving; similarly, separate medications are available to help improve the symptoms of depression and anxiety. More research is needed, however, to better understand how such medications act when combined in individuals with comorbidities, or whether such medications can be dually effective for treating comorbid conditions.
Mental Health Care among Adults with Co-Occurring Serious Mental Illness and Substance Use Disorders
- Among the 2.5 million adults aged 18 or older with both SMI and substance dependence or abuse (i.e., a substance use disorder) in 2008, 60.5 percent received mental health care or substance use treatment at a specialty facility; 11.4 percent received both mental health care and specialty substance use treatment, 45.2 percent received only mental health care, and 3.7 percent received only specialty substance use treatment.
Past Year Mental Health Care and Treatment for Substance Use Problems among Adults Aged 18 or Older with Both Serious Mental Illness and a Substance Use Disorder: 2008
Other Information Sources
For more information on comorbidity between drug use disorders and other mental illnesses, see—
National Institute of Mental Health, National Institutes of Health, at www.nimh.nih.gov
Substances:
Category and Name |
Examples of Commercial
and Street Names |
DEA Schedule/Administration Route |
Intoxication Effects/Potential Health Consequences |
Cannabinoids |
euphoria, slowed thinking and reaction time, confusion, impaired balance and coordination/cough, frequent respiratory infections; impaired memory and learning; increased heart rate, anxiety; panic attacks; tolerance, addiction |
hashish |
boom, chronic, gangster, hash, hash oil, hemp |
I/swallowed, smoked
|
marijuana |
blunt, dope, ganja, grass, herb, joints, Mary Jane, pot, reefer, sinsemilla, skunk, weed |
I/swallowed, smoked
|
Depressants |
reduced anxiety; feeling of well-being; lowered inhibitions; slowed pulse and breathing; lowered blood pressure; poor concentration/fatigue; confusion; impaired coordination, memory, judgment; addiction; respiratory depression and arrest; death
Also, for barbiturates—sedation, drowsiness/depression, unusual excitement, fever, irritability, poor judgment, slurred speech, dizziness, life-threatening withdrawal
for benzodiazepines—sedation, drowsiness/dizziness
for flunitrazepam—visual and gastrointestinal disturbances, urinary retention, memory loss for the time under the drug's effects
for GHB—drowsiness, nausea/vomiting, headache, loss of consciousness, loss of reflexes, seizures, coma, death
for methaqualone—euphoria/depression, poor reflexes, slurred speech, coma |
barbiturates |
Amytal, Nembutal, Seconal, Phenobarbital: barbs, reds, red birds, phennies, tooies, yellows, yellow jackets |
II, III, V/injected, swallowed
|
benzodiazepines (other than flunitrazepam) |
Ativan, Halcion, Librium, Valium, Xanax: candy, downers, sleeping pills, tranks |
IV/swallowed, injected
|
flunitrazepam |
Rohypnol: forget-me pill, Mexican Valium, R2, Roche, roofies, roofinol, rope, rophies |
IV/swallowed, snorted
|
GHB |
gamma-
hydroxybutyrate: G, Georgia home boy, grievous bodily harm, liquid ecstasy |
I/swallowed
|
methaqualone |
Quaalude, Sopor, Parest: ludes, mandrex, quad, quay |
I/injected, swallowed
|
Dissociative Anesthetics |
increased heart rate and blood pressure, impaired motor function/memory loss; numbness; nausea/vomiting
Also, for ketamine—at high doses, delirium, depression, respiratory depression and arrest
for PCP and analogs—possible decrease in blood pressure and heart rate, panic, aggression, violence/loss of appetite, depression |
ketamine |
Ketalar SV: cat Valiums, K, Special K, vitamin K |
III/injected, snorted, smoked
|
PCP and analogs |
phencyclidine; angel dust, boat, hog, love boat, peace pill |
I, II/injected, swallowed, smoked
|
Hallucinogens |
altered states of perception and feeling; nausea; persisting perception disorder (flashbacks)
Also, Also for LSD and mescaline—increased body temperature, heart rate, blood pressure; loss of appetite, sleeplessness, numbness, weakness, tremors
for for LSD—persistent mental disorders
for for psilocybin—nervousness, paranoia |
LSD |
lysergic acid diethylamide: acid, blotter, boomers, cubes, microdot, yellow sunshines |
I/swallowed, absorbed through mouth tissues
|
mescaline |
buttons, cactus, mesc, peyote |
I/swallowed, smoked
|
psilocybin |
magic mushroom, purple passion, shrooms |
I/swallowed
|
Opioids and Morphine Derivatives |
pain relief, euphoria, drowsiness/nausea, constipation, confusion, sedation, respiratory depression and arrest, tolerance, addiction, unconsciousness, coma, death
Also, for codeine—less analgesia, sedation, and respiratory depression than morphine
for heroin—staggering gait |
codeine |
Empirin with Codeine, Fiorinal with Codeine, Robitussin A-C, Tylenol with Codeine: Captain Cody, schoolboy; (with glutethimide) doors & fours, loads, pancakes and syrup |
II, III, IV, V/injected, swallowed
|
fentanyl and fentanyl analogs |
Actiq, Duragesic, Sublimaze: Apache, China girl, China white, dance fever, friend, goodfella, jackpot, murder 8, TNT, Tango and Cash |
I, II/injected, smoked, snorted
|
heroin |
diacetyl-
morphine: brown sugar, dope, H, horse, junk, skag, skunk, smack, white horse |
I/injected, smoked, snorted
|
morphine |
Roxanol, Duramorph: M, Miss Emma, monkey, white stuff |
II, III/injected, swallowed, smoked
|
opium |
laudanum, paregoric: big O, black stuff, block, gum, hop |
II, III, V/swallowed, smoked
|
oxycodone HCL |
Oxycontin: Oxy, O.C., killer |
II/swallowed, snorted, injected
|
hydrocodone bitartrate, acetaminophen |
Vicodin: vike, Watson-387 |
II/swallowed
|
Stimulants |
increased heart rate, blood pressure, metabolism; feelings of exhilaration, energy, increased mental alertness/rapid or irregular heart beat; reduced appetite, weight loss, heart failure, nervousness, insomnia
Also, for amphetamine—rapid breathing/tremor, loss of coordination; irritability, anxiousness, restlessness, delirium, panic, paranoia, impulsive behavior, aggressiveness, tolerance, addiction, psychosis
for cocaine—increased temperature/chest pain, respiratory failure, nausea, abdominal pain, strokes, seizures, headaches, malnutrition, panic attacks
for MDMA—mild hallucinogenic effects, increased tactile sensitivity, empathic feelings/impaired memory and learning, hyperthermia, cardiac toxicity, renal failure, liver toxicity
for methamphetamine—aggression, violence, psychotic behavior/memory loss, cardiac and neurological damage; impaired memory and learning, tolerance, addiction
for nicotine—additional effects attributable to tobacco exposure; adverse pregnancy outcomes; chronic lung disease, cardiovascular disease, stroke, cancer, tolerance, addiction |
amphetamine |
Biphetamine, Dexedrine: bennies, black beauties, crosses, hearts, LA turnaround, speed, truck drivers, uppers |
II/injected, swallowed, smoked, snorted
|
cocaine |
Cocaine hydrochloride: blow, bump, C, candy, Charlie, coke, crack, flake, rock, snow, toot |
II/injected, smoked, snorted
|
MDMA (methylenedioxy-
methamphetamine) |
Adam, clarity, ecstasy, Eve, lover's speed, peace, STP, X, XTC |
I/swallowed
|
methamphetamine |
Desoxyn: chalk, crank, crystal, fire, glass, go fast, ice, meth, speed |
II/injected, swallowed, smoked, snorted
|
methylphenidate (safe and effective for treatment of ADHD) |
Ritalin: JIF, MPH, R-ball, Skippy, the smart drug, vitamin R |
II/injected, swallowed, snorted
|
nicotine |
cigarettes, cigars, smokeless tobacco, snuff, spit tobacco, bidis, chew |
not scheduled/smoked, snorted, taken in snuff and spit tobacco
|
Other Compounds |
anabolic steroids |
Anadrol, Oxandrin, Durabolin, Depo-
Testosterone, Equipoise: roids, juice |
III/injected, swallowed, applied to skin
|
no intoxication effects/hypertension, blood clotting and cholesterol changes, liver cysts and cancer, kidney cancer, hostility and aggression, acne; in adolescents, premature stoppage of growth; in males, prostate cancer, reduced sperm production, shrunken testicles, breast enlargement; in females, menstrual irregularities, development of beard and other masculine characteristics |
Dextromethorphan (DXM) |
Found in some cough and cold medications; Robotripping, Robo, Triple C |
not scheduled/swallowed
|
Dissociative effects, distorted visual perceptions to complete dissociative effects/for effects at higher doses see 'dissociative anesthetics' |
inhalants |
Solvents (paint thinners, gasoline, glues), gases (butane, propane, aerosol propellants, nitrous oxide), nitrites (isoamyl, isobutyl, cyclohexyl): laughing gas, poppers, snappers, whippets |
not scheduled/inhaled through nose or mouth
|
stimulation, loss of inhibition; headache; nausea or vomiting; slurred speech, loss of motor coordination; wheezing/unconsciousness, cramps, weight loss, muscle weakness, depression, memory impairment, damage to cardiovascular and nervous systems, sudden death |
|
Contact us for info. <> Most Insurance Accepted
2724-8 Capital Circle NE, FL 32308, Ph: 850.656.5112 <> Fx: 850.656.3802

|
|
